Accessing sleep data to assess appropriate use of antipsychotics
The Sleep Score offers caregivers a non-bias method to assess medication changes
Overview
A recent study has revealed an increase in antipsychotic drugs use in long-term care homes across Canada despite no significant increase in behavioural symptoms of residents – something that may expose a potential area of concern for quality of care, researchers say. The study, published in Health Services Insights, examined data from yearly Canadian Institute for Health Information (CIHI) reports to assess how COVID-19 impacted resident admission and discharge rates, resident health attributes, treatments, and quality of care. According to CAMH, these drugs have unpleasant side effects, including dizziness (which increases the risk of falls), weight gain, and diabetes, most of which will go away after stopping drug use.
While many senior care providers are determined to reduce the amount of antipsychotics prescribed to seniors in long term care, there has not been a method, until now, by which to assess the effects of tapering down a senior’s prescription. This case study shows how Sleepsense is able to provide data driven feedback in accessing the appropriate use of antipsychotics for a resident.
Langley Lodge a long-term care home in BC received a new resident who was clinically diagnosed with psychosis, dementia and hypertension. This resident who continually resisted care and was deemed to not be coping well, was on a lot of antipsychotic medication including risperidone TID(0900, 1200, 2000) prior to arrival. After a few months, care staff at Langley Lodge worked with a nurse practitioner to reduce the resident’s antipsychotic medications use. Sleepsense was used as a means to assess the impact of the tapering down of antipsychotics for the resident. The resident’s Sleep Scores and her behaviour were continuously reviewed over several months as care staff tapered down antipsychotic dosage until it was eventually discontinued altogether.
The Sleepscores of the resident pre-intervention and post-intervention showed no change indicating the antipsychotics the resident was taking did not result in her having a better sleep. She was sleeping just as well without the medication.
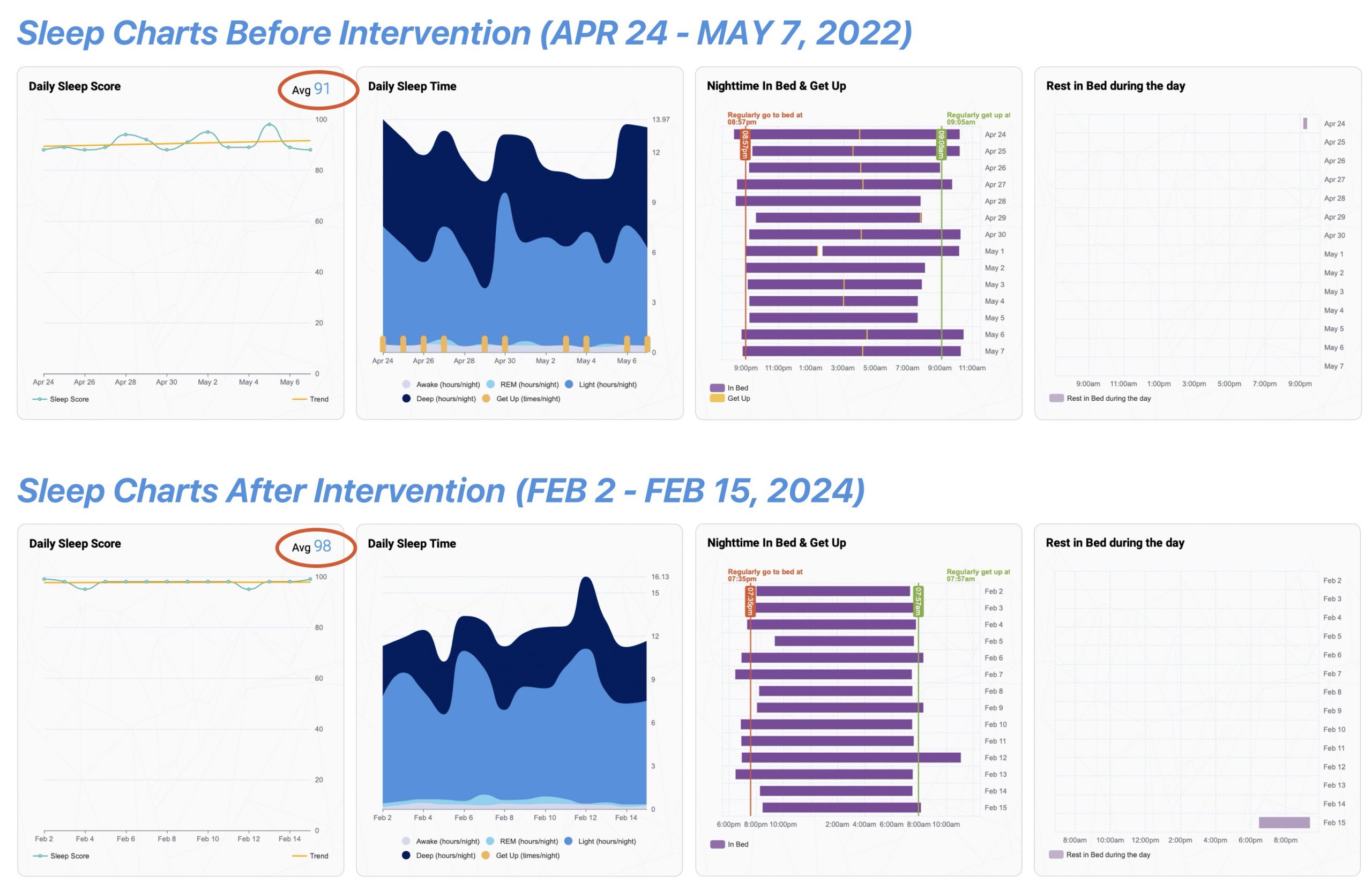
Sleep scores pre and post intervention remain unchanged.
Impact
Reduction in use of antipsychotics
Medication changes based on unbiased data
Improved quality of life from reduced medication side effects
Key Takeaways
Sleepsense provides care staff with the information to make informed decisions when reducing antipsychotic medication.
-
Sleepsense provides unbiased sleep data offers care providers the confidence to make appropriate medication changes that will positively the quality of life of residents.
